Managing procedural anxiety in children: reframe the pain

Anxiety is increasingly prevalent in children. GPs play an important role in identifying and targeting anxiety prior to medical procedures for optimal pain management. The behaviours of parents and caregivers also influence children’s procedural anxiety, suggesting the need for family-centred approaches and supportive parental behaviour preparation programs. Reframing communication and implementing distraction aids can help reduce procedural anxiety in children.
- Procedural anxiety in children can be identified through risk assessment, including underlying anxiety disorders, developmental disorders and previous negative experiences.
- Behaviour preparation programs can improve procedural outcomes by mitigating anxiety, distress and analgesic usage and facilitating early discharge.
- Parental anxiety and distress influence a child’s anxiety and pain during medical procedures, highlighting the need for family-centred interventions and parental behaviour training.
- Appropriate communication strategies, simple interventions, distraction aids and the avoidance of physical restraint contribute to managing procedural anxiety effectively.
The diagnosis of anxiety in children by paediatricians is on the rise. A study examining trends in the prevalence of childhood anxiety in Australia found an almost twofold increase in anxiety diagnoses accompanied by an increase in the prescription of anxiety medications between 2008 and 2013.1 The levels of anxiety in children and adolescents are significantly higher since the COVID-19 pandemic.2 We are likely to see more highly anxious children presenting for procedural care, many of whom will be young. The positive correlations among state and trait anxiety and pain intensity, analgesic consumption and functional disability are well recognised in children.3-6 Anxiety is the most significant predictor of postoperative pain severity.7 This article describes the importance of identifying and targeting anxiety prior to procedural care to optimise pain management. The role of parents and caregivers in influencing a child’s anxiety and distress during medical procedures is also highlighted, suggesting the need for family-centred interventions and supportive parental behaviour training.
Identifying procedural anxiety in children
For optimal pain management in children, potentially modifiable psychological factors, such as anxiety, should be identified, assessed and targeted prior to procedural care.4,7 Formal risk assessment for anxiety is impractical at the point of care. However, clinicians can identify children who may be at increased risk. Children with an underlying anxiety disorder, such as generalised anxiety disorder, social anxiety disorder or selective mutism, can be identified on the basis of a careful history. Those with developmental disorders associated with anxiety, such as autism spectrum disorder and ADHD, can also be readily identified and assessed. Children may present with a pre-existing procedure-related specific phobia, such as blood injury phobia or mask phobia. Children who have undergone procedures and those with underlying chronic medical conditions are at an increased risk of procedure-related fear or phobia. Exploring a child’s response to previous procedures is important for identifying and assessing this risk group.
Behaviour preparation programs for procedural care
Behaviour preparation programs for procedural care improve perioperative outcomes by reducing anxiety and distress, analgesic usage and postoperative delirium, as well as facilitating early discharge.8-10 Previously, behaviour preparation programs were considered time consuming and costly compared with preprocedural sedation with drugs, such as midazolam.10 However, as we encounter increasing numbers of highly anxious children and greater numbers of failed procedures, and as we gain a better understanding of the long-term negative impact of procedural distress and pain, procedural preparation is becoming a vital service that should be offered to at-risk children and their families. Children benefit from receiving clear procedural and sensory information commensurate with their age and should therefore be informed about the upcoming procedures and what they can expect to experience.8 Children should also be offered training in coping techniques, such as distraction and deep breathing.8
Parental anxiety
Parental anxiety and pain catastrophising are associated with increased pain intensity and analgesic usage, which in turn are predictive of acute and chronic postoperative pain in children.5,11 Parental anxiety and traumatic stress symptoms influence children’s coping and distress behaviours during procedures, through distress-promoting behaviours in parents.12,13 Therefore, parental anxiety is a major modifiable risk factor of children’s anxiety and pain, and screening for caregiver anxiety is recommended to identify children at risk of developing procedural anxiety.7,11,13-15
Children rely on their parents and caregivers for emotional co-regulation and the interpretation of threat and harm. During unfamiliar and stressful medical procedures, children are acutely aware of, and respond to, parental cues.16 Therefore, parents and carers play a pivotal role in a child’s perception of pain and the psychological recovery following negative experiences.14 A parent who is anxious or distressed will be unavailable to the child in the acute phase of a procedure and, importantly, in the period following the procedure due to their own withdrawal and avoidance. Parental behaviour training programs reduce a child’s distress related to painful procedures.17 Given the recognised interplay between parental and child anxiety and pain, interventions aimed at reducing a child’s traumatic stress reactions must be considered in the context of the parent–child relationship and should be family centred.14
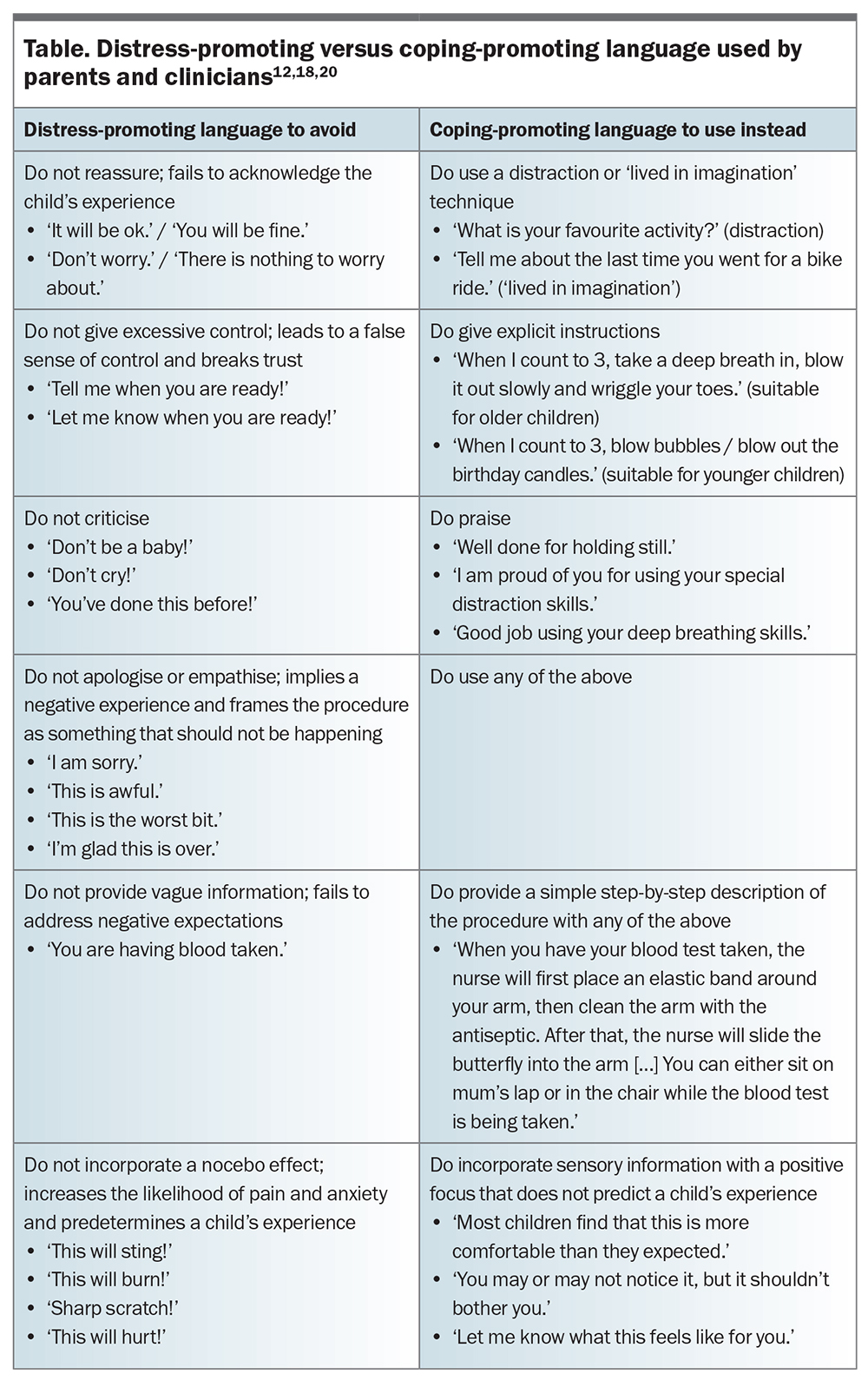
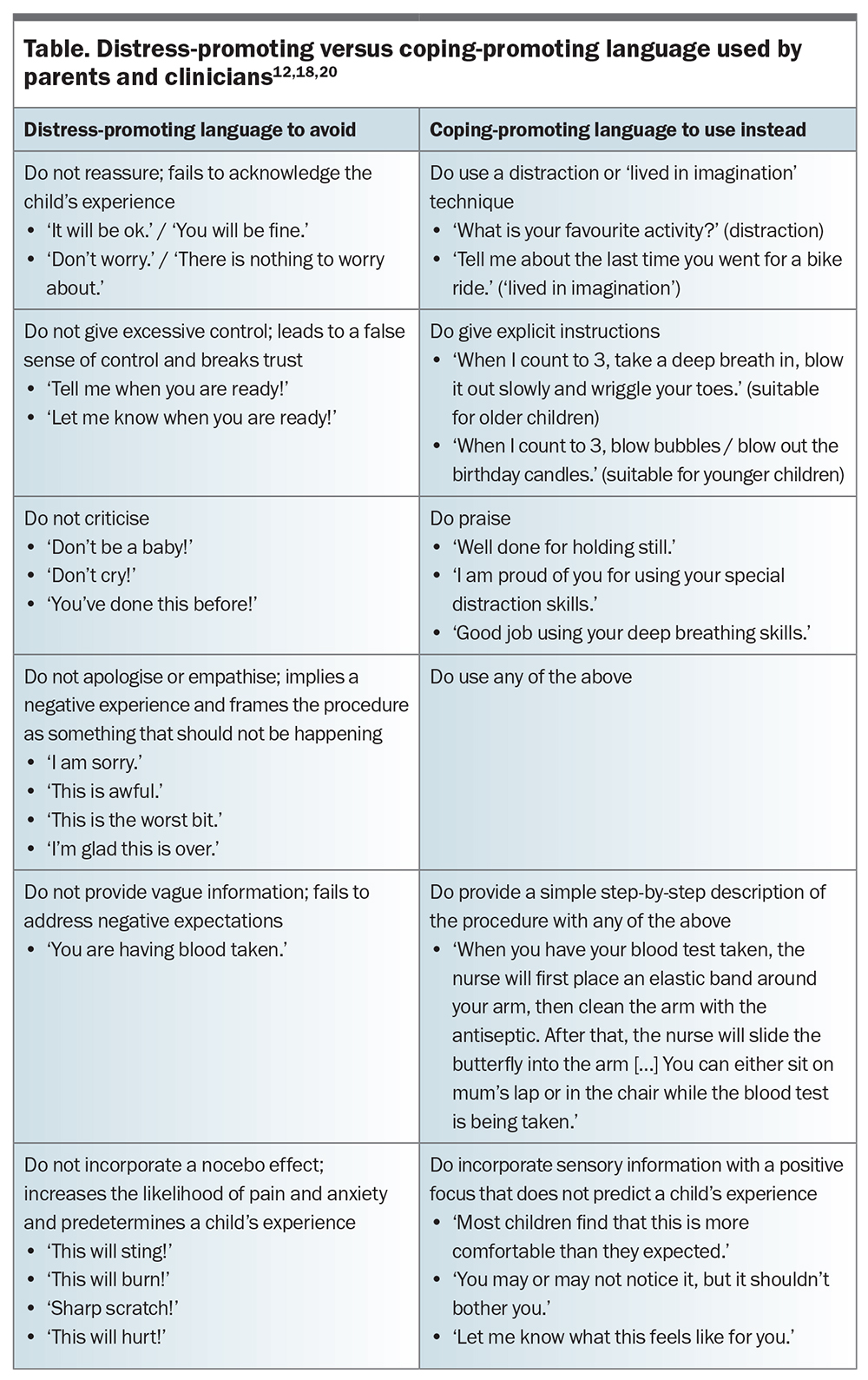
Parental behaviours that are associated with children’s distress have been identified. Procedural distress in children is promoted when parents provide negative information or use excessive reassurance, empathy and criticism. Apologising and giving control to the child also promote distress.13,18,19 Parental behaviour that involves nonprocedure-related communication, distractions (such as humour) and specific coping strategies (such as deep breathing techniques) improves children’s ability to cope with medical procedures.13,20 These coping-promoting and distress-promoting parental behaviours have been incorporated into validated scales such as the Child-Adult Medical Procedure Interaction Scale-Revised (CAMPIS-R). Modifications of the CAMPIS-R scale that include nonverbal behaviours have been validated for use in cases of burns and in the perioperative setting.16,17 Parents can be trained in appropriate language and strategies to support adaptive coping in children undergoing procedures (Table).12,18,20 Procedural preparation of parents and their children is now considered best practice.7
Placebo, nocebo and expectancy
Many studies have led to recommendations for assessing and targeting procedural anxiety to optimise pain management. However, there is little guidance on how clinicians can address this. To shed light on potential strategies for managing procedural anxiety, we can turn to the literature on placebo, nocebo and expectancy in clinical practice. Placebo effects are the psychobiological effects that occur as a result of the psychosocial context surrounding the patient, which includes memory, prior learning, expectancy and conditioning.7 Nocebo describes negative psychobiological effects resulting from the psychosocial context.7 Placebo and nocebo effects occur in routine clinical care, and ethical harnessing of placebo effects and minimisation of nocebo effects can improve the outcomes of clinical interventions.7,21,22 Placebo and nocebo effects strongly influence analgesic efficacy, with pain studies showing moderate to large effects.7 Expectancy is a powerful determinant of placebo responses to analgesic agents.21 Positive expectancy can increase analgesic efficacy by more than twofold, whereas negative expectancy can completely abolish the analgesic effect of potent drugs, such as remifentanil.7,21-23 Expectancy should therefore be assessed and modulated throughout treatment.7
Managing procedural anxiety
Communication strategies
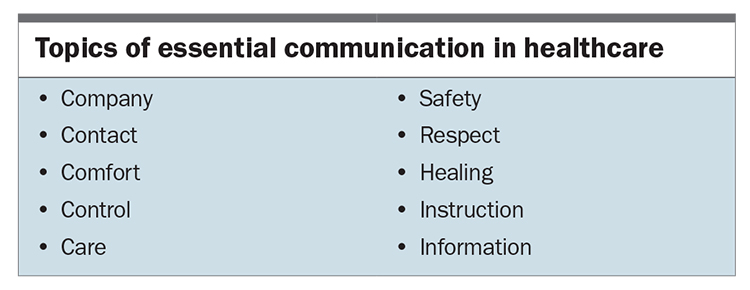
Minor changes in how information is communicated to patients can significantly alter expectancy and the magnitude of placebo and nocebo effects.7 The addition of meaning to communicated information is a simple means of modulating expectancy, thereby increasing the effectiveness of therapy.22 The Box lists topics of essential communication in healthcare, which are derived from humans’ basic psychological needs and factors that contribute to the development of post-traumatic stress. These topics should be reiterated as often as possible throughout a patient’s journey, thereby increasing positive expectancy and counteracting the impact of negative suggestions and nocebo effects to which the patient is exposed.22 For example, by way of introduction, an anaesthetist might say to a child: ‘I am the doctor who takes care of you while you have your operation. That means that I drift you off to sleep, keep you safe and comfortable during the procedure and allow you to wake up safely at the end. I will be with you, monitoring your safety and comfort all the time until the operation is finished’.
Children should be treated with respect and allowed a sense of control where possible. They should also be given accurate information and clear instructions, commensurate with their age. Many clinicians struggle with providing risk information, aware that such information can be distressing to children. Clinicians can reframe the potential negative impact of risk information by combining this information with positive aspects, such as the benefits of therapy or steps taken to minimise the risk.22 For example, when explaining the risk of aspiration, one can praise a child for having fasted appropriately prior to sedation or anaesthesia, thereby contributing to keeping themselves as safe as possible from this risk. In this way, risk is reframed as safety. Attention can then be shifted from hunger to the successful completion of the procedure by asking the child what they would like to eat after the procedure is completed.
Interventions and distraction aids
Immersive virtual reality can reduce self-reported anxiety during medical procedures.7 Music therapy can alleviate pain and anxiety during procedures involving the use of needles. The addition of passive music to standard care for intravenous cannulation can reduce both pain and anxiety scores.7 Hypnosis for procedures involving the use of needles can reduce pain and distress scores.7 Although formal hypnosis is performed by trained practitioners, hypnosis-based techniques for procedural pain and distress management can be learned through short training courses.
Positioning
Positioning is a simple manoeuvre that can modify distress. Sitting up is less distressing than lying down, and being held by a parent is associated with less distress compared with being restrained by medical staff. Restraining children for medical procedures, defined as forcibly holding children against their wishes, creates a negative experience that can be more distressing than the procedure itself. Restraint can lead to long-term negative psychosocial effects.24 Children with mask or needle phobia often report a single incident where restraint was used. Participation in restraint can leave parents with feelings of guilt, disempowerment, anger and a loss of trust in healthcare professionals.25 Parental guilt is a factor in mediating procedural anxiety and distress in children.14 Where possible, physical restraint for medical procedures should be avoided.
Practice points for procedural preparation
Procedural anxiety results in increased pain, physical restraint, failed procedures and avoidance of medical care. Baseline variables such as an anxious temperament, a negative experience in the past and the presence of developmental disorders that influence a child’s anxiety are less amenable to modification at the point of care.17 Procedural preparation should be offered to all children, with those at increased risk being offered more specialised care by clinicians, such as child life therapists. Factors arising at the time of performing painful procedures, such as the behaviours of medical staff and parents, are amenable to modification.17 Parental presence is routinely implemented to reduce child distress. However, anxious or distressed parents display parental behaviours that promote distress and reduce a child’s coping ability. Anxious parents require additional support and training for their presence to be beneficial.13 A family-centred approach to behavioural preparation should be adopted.
The same patterns of distress-promoting behaviours displayed by parents are often displayed by clinicians.26 Clinicians can be trained in the effective use of coping-promoting behaviours and reframing language techniques. They are encouraged to be trained in effective procedural communication that emphasises the positive effects of treatment, avoids focusing on the negative effects and manages expectations through careful explanation (Table).12,18,20,22,27 Clinicians are encouraged to foster a clinician–patient relationship characterised by warmth, trust and empathy.27 This form of empathic engagement has been termed the ritual of the therapeutic act. It is at the heart of placebo and nocebo responses and is an important and measurable component of therapeutic responses.21
Conclusion
Addressing procedural anxiety requires a comprehensive approach that includes proactive procedural preparation for all children and specialised care for those at increased risk. Modifying the behaviours of medical staff and parents when a child is undergoing a procedure is essential, as anxious parents and clinicians can inadvertently promote distress in children. Implementing coping-promoting behaviours and effective procedural communication, and fostering a compassionate clinician–patient relationship, are key elements in mitigating procedural anxiety and optimising therapeutic outcomes. PMT
COMPETING INTERESTS: None.
References
1. Danchin M, Gulenc A, Efron D, Sciberras E, Symeonides C, Hiscock H. Trends in prevalence and management of childhood anxiety by Australian pediatricians. Acad Pediatr 2019; 19: 35-43.
2. Wang S, Chen L, Ran H, et al. Depression and anxiety among children and adolescents pre and post COVID-19: a comparative meta-analysis. Front Psychiatry 2022; 13: 917552.
3. Chieng YJS, Chan WCS, Liam JLW, Klainin-Yobas P, Wang W, He HG. Exploring influencing factors of postoperative pain in school-age children undergoing elective surgery. J Spec Pediatr Nurs 2013; 18: 243-252.
4. Chieng YJS, Chan WCS, Klainin-Yobas P, He HG. Perioperative anxiety and postoperative pain in children and adolescents undergoing elective surgical procedures: a quantitative systematic review. J Adv Nurs 2014; 70: 243-255. 5. Chow CHT, Schmidt LA, Buckley DN. The role of anxiety and related states in pediatric postsurgical pain. Can J Pain 2020; 4: 26-36.
6. Pagé G, Stinson, Campbell, Isaac, Katz J. Pain-related psychological correlates of pediatric acute post-surgical pain. J Pain Res 2012; 5: 547-548.
7. Schug SA, Palmer GM, Scott DA, Alcock M, Halliwell R, Mott J, eds. Acute pain management: scientific evidence. 5th ed. Melbourne: Australian and New Zealand College of Anaesthetists; 2020.
8. Chorney JM, Kain ZN. Family-centered pediatric perioperative care. Anesthesiology 2010; 112: 751-755.
9. Davidson A, Mckenzie I. Distress at induction: prevention and consequences. Curr Opin Anaesthesiol 2011; 24: 301-306.
10. Kain ZN, Caldwell-Andrews AA, Mayes LC, et al. Family-centered preparation for surgery improves perioperative outcomes in children: a randomized controlled trial. Anesthesiology 2007; 106: 65-74.
11. Oommen S, Shetty A. Does parental anxiety affect children’s perception of pain during intravenous cannulation? Nurs Child Young People 2020; 32: 21-24.
12. Brown EA, De Young A, Kimble R, Kenardy J. The role of parental acute psychological distress in paediatric burn re-epithelialization. Br J Health Psychol 2019; 24: 876-895.
13. Brown EA, De Young A, Kimble R, Kenardy J. Impact of parental acute psychological distress on young child pain-related behavior through differences in parenting behavior during pediatric burn wound care. J Clin Psychol Med Settings 2019; 26: 516-529.
14. de Young AC, Hendrikz J, Kenardy JA, Cobham VE, Kimble RM. Prospective evaluation of parent distress following pediatric burns and identification of risk factors for young child and parent posttraumatic stress disorder. J Child Adolesc Psychopharmacol 2014; 24: 9-17.
15. Knoetze R, Lachman A, Moxley K, Chetty S. Caregiver anxiety and the association with acute postoperative pain in children undergoing elective ambulatory surgery in a lower-middle-income country setting. Cravero J, ed. Pediatr Anaesth 2020; 30: 990-997.
16. Brown EA, De Young A, Kimble R, Kenardy J. Development and validity of the Burns-Child Adult Medical Procedure Interaction Scale (B-CAMPIS) for young children. Burns 2019; 45: 76-87.
17. Caldwell-Andrews AA, Blount RL, Mayes LC, Kain ZN. Behavioral interactions in the perioperative environment. Anesthesiology 2005; 103: 1130-1135.
18. Cyna AM. Little words BIG impact: perioperative communication for children with burns. Anaesth Intensive Care 2020; 48: 123-128.
19. Cyna AM, Andrew MI, Tan SGM. Communication skills for the anaesthetist. Anaesthesia 2009; 64: 658-665.
20. Krauss BS, Krauss BA, Green SM. Managing procedural anxiety in children. N Engl J Med 2016; 374: e19.
21. Benedetti F. Placebo and the new physiology of the doctor-patient relationship. Physiol Rev 2013; 93: 1207-1246.
22. Hansen E, Zech N. Nocebo effects and negative suggestions in daily clinical practice – forms, impact and approaches to avoid them. Front Pharmacol 2019; 10: 77.
23. Bingel U, Wanigasekera V, Wiech K, et al. The effect of treatment expectation on drug efficacy: imaging the analgesic benefit of the opioid remifentanil. Sci Transl Med 2011; 3: 70ra14.
24. Bray L, Snodin J, Carter B. Holding and restraining children for clinical procedures within an acute care setting: an ethical consideration of the evidence. Nurs Inq 2014; 22: 157-167.
25. Bray L, Carter B, Snodin J. Holding children for clinical procedures: perseverance in spite of or persevering to be child-centered. Res Nurs Health 2016; 39: 30-41.
26. Chorney JM, Torrey C, Blount R, McLaren CE, Chen WP, Kain ZN. Healthcare provider and parent behavior and children’s coping and distress at anesthesia induction. Anesthesiology 2009; 111: 1290-1296.
27. Evers AWM, Colloca L, Blease C, et al. Implications of placebo and nocebo effects for clinical practice: expert consensus. Psychother Psychosom 2018; 87: 204-210.